Written by Brian Shilhavy
Editor, Health Impact News
Recently we covered a study published in the journal Clinical Nutrition which compared peanut oil consumption with coconut oil consumption among healthy men in India, where those who consumed coconut oil had better health outcomes in terms of heart disease and diabetes.
A researcher at The University of Edinburgh Medical School wrote a Letter to the Editor of Clinical Nutrition commenting on this study, criticizing current government nutritional guidelines regarding saturated dietary fat restrictions.
The cross-over study by Korrapati et al. detailed the potential cardioprotective effect of coconut oil, and I would like to thank the authors for their insight. Whilst the sample size was small, it was well-designed to investigate its primary end-points.
This study is particularly topical as, despite removal of the maximum dietary fat intake restriction from guidelines, a major resistance against saturated fats remains.
Setting aside the issue of whether or not saturated fats should be restricted at all, given the abundance of contrary evidence in the medical literature, the Edinburgh Medical School researcher reported that such guidelines do not distinguish between different types of saturated fats. Saturated fats can be found in animal products, such as butter, as well as plant sources, such as coconuts and date palms.
The rise in high density lipoprotein cholesterol (HDL-c) with coconut oil consumption is certainly a compelling finding. Results from a recent and larger-scale randomised trial by Khaw et al. corroborate this, but, interestingly, a similar HDL-c elevation was not seen with butter intake, which is also largely composed of saturated fatty acids (SFAs). Indeed, accruing evidence suggests that the saturated versus unsaturated distinction of fats is likely an oversimplification.
Korrapati et al. should, therefore, be commended on their focus on the biological properties of coconut oil, particularly the medium chain triglyceride (MCT) dominated fatty acid profile, which may confer atheroprotective effects.
Of note, a recent UK/Danish cohort study elicited that chain length is a major determinant of SFA-associated myocardial infarction risk, with no delineable, or even an inverse, relationship existing with short-tomedium chain SFA consumption.
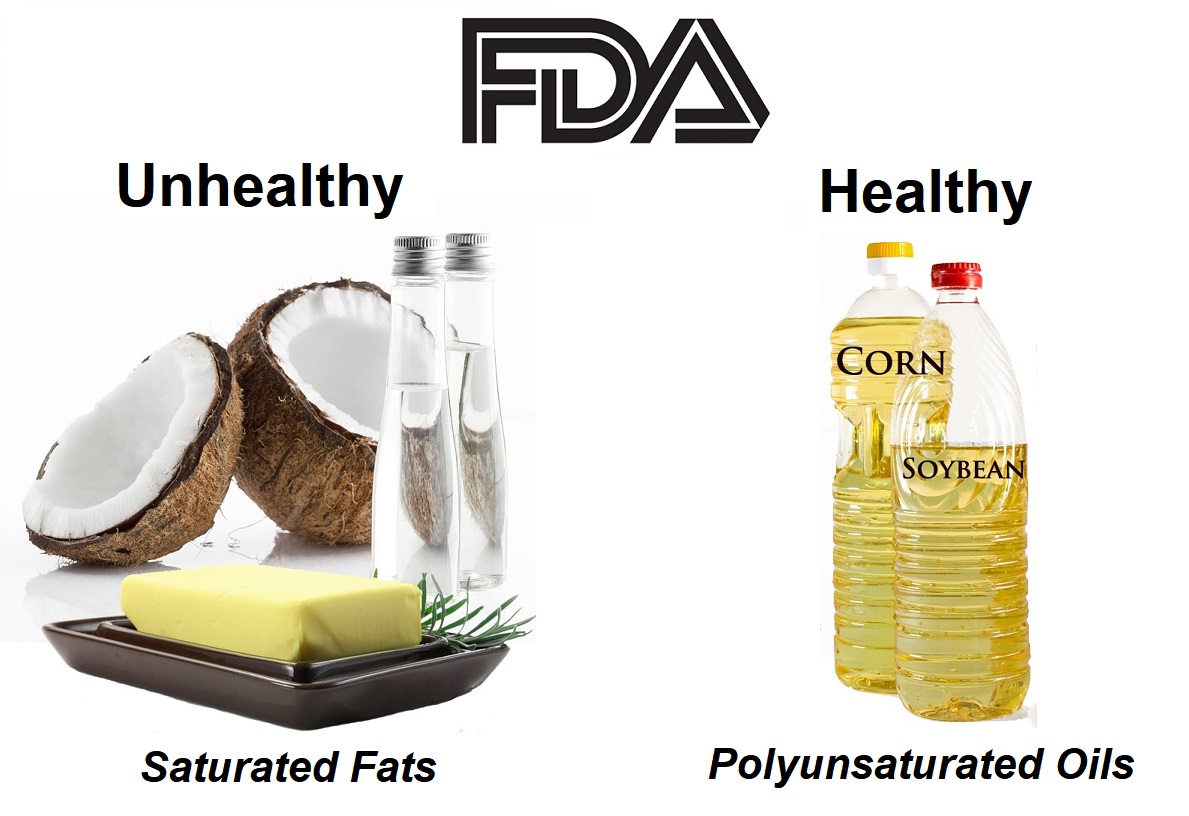
The researcher also noted the inherent problems with most government nutritional guidelines to replace saturated fats with polyunsaturated fats that are supposed to be more “heart healthy,” when polyunsaturated fats are prone to lipid peroxidation which make them toxic, and are linked to inflammatory causes.
RELATED:
The promotion of polyunsaturated oils (mostly corn and soybean oils in western countries, but sometimes peanut oil in Asian countries like this study) in the modern day diet also leads to an Omega 6 to Omega 3 ratio imbalance.
I note that the detrimental impacts of peanut oil consumption were comparatively overlooked in the analysis; it would have been interesting to explore the authors’ interpretation of this data.
The unfavourable lipid profile, with elevation of low-density lipoprotein cholesterol (LDL-c), is an especially salient finding given the long-standing recommendations to substitute polyunsaturated fatty acids (PUFAs) in place of SFAs.
It is difficult to discern from the methodology whether the additional 35 g of coconut/peanut oil daily was provided in a cold formulation, or whether it was heated for meal preparation.
With a significantly greater PUFA content than coconut oil, peanut oil is more susceptible to lipid peroxidation during cooking; numerous studies have demonstrated a deranged metabolic profile, including elevated inflammatory markers and LDL-c, with hot vegetable oil intake [5], and, thus, clarification on this issue would be greatly appreciated.
Furthermore, whilst Korrapati et al. outline the 15-fold greater concentration of linoleic acid in peanut oil versus coconut oil, I wonder if this could have been further developed.
Linoleic acid represents the most abundant omega-6 fatty acid, and whilst no consensus has been reached regarding its contribution to cardiovascular disease, omega-3/omega-6 imbalance is becoming an increasingly contentious issue.
RELATED:
USDA Dietary Advice on Saturated Fats Based on Faulty or Corrupt Research
The “lipid theory” of heart disease, the theory that blames saturated fat and cholesterol for causing heart disease, is widely believed to be linked to a researcher in the late 1950s and early 1960s by the name of Ancel Keys from the University of Minnesota.
His original study has been shown to be false, with selective bias being used to only select certain populations that fit his theory.
Journalist Paul John Scott, writing for the Star Tribune in 2011, admitted that Keys’ work was not widely accepted by scientists at the time, and now is considered “junk science.”
We told the world that heart disease is caused by elevated cholesterol and that reducing saturated fat in the diet reduces this risk. That led the country to embrace the lowering of cholesterol with medications. All of those assumptions have proven themselves to be either overstated, oversimplified or wrong, and that has led us astray. Would it be too much for the leading cardiologists in our community to admit as much?
“It was also nearly 60 years ago,” as Dr. Daniel J. Garry extolled on these pages (“Treating heart disease at the U: A story of steady innovations,” April 14), “that University of Minnesota scientists — Dr. Ancel Keys along with Drs. Francisco Grande and Joseph Anderson — defined the relationship between dietary fat and serum cholesterol, which linked cholesterol to heart disease.”
Garry went on to praise the creation of cholesterol-lowering drugs that stemmed from Keys’ work. Keys constructed his hypothesis after studying the diets and heart disease in countries across the globe. But his research left out nations with data that did not match the hypothesis, and even within the data he published, populations existed in which diet and heart disease were wildly out of synch with his model.
By 1970, an English researcher named John Yudkin would argue that sugar in the diet was the cause of heart disease in wealthy nations, but Keys, sensing that his theory was suddenly vulnerable to reconsideration, aggressively led the charge to have that research discredited.
Nevertheless, this faulty research was used during the 1970s in a Congressional hearing to decide USDA nutritional advice in, and the infamous “McGovern Report” on nutrition resulted in condemning saturated fats and blaming them for causing heart disease, even over the objections of many scientists who did not believe Keys’ research.
This YouTube clip contains actual film footage by ABC news regarding the McGovern report in 1977, and how scientists cautioned the politicians at that time that the science did NOT support the conclusion that saturated fats and cholesterol caused heart disease.
In 2017, a group of researchers with the Philip R. Lee Institute for Health Policy Studies at the University of California at San Francisco (UCSF), reviewed historical scientific literature funded by the Sugar Research Foundation since the 1960s, which gives us a great perspective on how the war on saturated fats became public policy.
These researchers at UCSF, Cristin E. Kearns, DDS, MBA; Laura A. Schmidt, PhD, MSW, MPH; and Stanton A. Glantz, PhD, revealed how the Sugar Research Foundation (SRF) influenced Harvard medical researchers financially and otherwise to report open-ended inconclusive research that omitted a lot of conclusive negative health data.
Their first article was published in the Journal of the American Medical Association (JAMA Internal Medicine) in 2016.
The title of the study is Sugar Industry and Coronary Heart Disease Research: A Historical Analysis of Internal Industry Documents.
The New York Times, which has given some press to exposing the saturated fat myth for over ten years now, led the mainstream media outlets that covered the UCSF study:
RELATED:
How the Sugar Industry Shifted Blame to Fat
Here are some excerpts:
The sugar industry paid scientists in the 1960s to play down the link between sugar and heart disease and promote saturated fat as the culprit instead, newly released historical documents show.
The internal sugar industry documents, recently discovered by a researcher at the University of California, San Francisco, and published Monday in JAMA Internal Medicine, suggest that five decades of research into the role of nutrition and heart disease, including many of today’s dietary recommendations, may have been largely shaped by the sugar industry.
“They were able to derail the discussion about sugar for decades,” said Stanton Glantz, a professor of medicine at U.C.S.F. and an author of the JAMA Internal Medicine paper.
The documents show that a trade group called the Sugar Research Foundation, known today as the Sugar Association, paid three Harvard scientists the equivalent of about $50,000 in today’s dollars to publish a 1967 review of research on sugar, fat and heart disease. The studies used in the review were handpicked by the sugar group, and the article, which was published in the prestigious New England Journal of Medicine, minimized the link between sugar and heart health and cast aspersions on the role of saturated fat.
Even though the influence-peddling revealed in the documents dates back nearly 50 years, more recent reports show that the food industry has continued to influence nutrition science.
The UCSF researchers disclosed how a top executive, John Hickson, vice-president of the SRF at the time took on the task of finding a way to discredit the increasing studies demonstrating sugar’s role in creating bad heart health.
Interestingly, a few years later in the early 1970s, Hickson became part of the tobacco industry’s PR machinery with the Cigar Research Council.
“In 1972, an internal tobacco industry memo on Mr. Hickson noted that he had a reputation for manipulating science to achieve his goals,” and “ …[he is] a supreme scientific politician who had been successful in condemning cyclamates [earlier artificial sweeteners], on behalf of the Sugar Research Council, on somewhat shaky evidence.”
Hickson had come up the idea of funding their own research which would enable them to legitimately and officially discredit all the anti-health sugar conclusions.
The operational key for this scheme was in Harvard, where “one of the researchers was the chairman of Harvard’s Public Health Nutrition Department — and an ad hoc member of SRF’s board.”
Their review was published in a 1967 issue of the New England Journal of Medicine.
The fact that it was published in such a prestigious journal as a scientific literature review was enough to establish legitimacy, at least enough to confuse, if not convince, with their inconclusive commentaries of “further studies needed.”
The review also maintained the now debunked lipid theory of heart disease by encouraging a low fat diet, which led to the McGovern Report.
FDA Prohibits Free Speech on Coconut Oil – Illegal to Call it “Healthy”
After the McGovern Report condemned saturated fats as “bad” and causing high cholesterol levels leading to heart disease, the FDA enacted rules for nutritional labeling and a recommended daily limit to consuming saturated fats.
If any product contains more than their recommended daily limit, that product cannot be labeled as “healthy.”
Since coconut oil is over 90% saturated, although with medium chain fatty acids that an abundance of scientific studies show are health promoting, it can never be marketed as “healthy.”
I learned this first hand in 2005, just 3 years after starting my company Tropical Traditions, the first company to import and sell a “virgin” coconut oil product from the Philippines.
Consumers from all over the U.S. were discovering just how healthy virgin coconut oil was, and we published their testimonies along with peer-reviewed scientific studies backing the claims.
But the FDA issued us a warning letter stating that we were selling “unapproved drugs” since they had not sanctioned or approved any of these claims, in spite of the abundance of testimonials and scientific studies.
Since we did not have the funds to go through the drug approval process, which can cost billions of dollars, and since the FDA has never approved of a natural substance that cannot be patented as a “drug,” we were forced to remove all testimonials and links to the scientific literature from the website where we were selling coconut oil.
This FDA rule is being used by attorneys who specialize in class action lawsuits to sue companies who sell coconut oil and market it as “healthy.”
Coconut Oil is a Threat to U.S. Subsidized Edible Oils and Big Pharma’s Cholesterol Drugs
Coconut oil is derived from coconuts, and must be imported as it is not produced much in the U.S.
Due to its growth in popularity in recent years, it can be seen as a threat to the edible oil industry and the pharmaceutical industry.
The United States is the world’s largest supplier of polyunsaturated edible oils, derived mainly from corn and soybeans, two very highly subsidized crops. As a result, the U.S. dominates the worldwide edible oil industry with these “vegetable oils.”
The concerted attack against saturated fats led to the industrial processing of corn and soy into edible oils. These are not traditional oils that have been in the food chain prior to WWII, as expeller-pressed technology was needed to extract oil from these crops.
These crops need to be chemically processed to remain shelf-stable as a dietary oil, and over 90% of the crops of corn and soy in the U.S. are from GMO seeds.
USDA dietary advice promotes polyunsaturated oils as “heart healthy,” in spite of strong evidence to the contrary.
In 2013 a report published in the British Medical Journal looked at resurrected data from a 1960s study, the Sydney Diet Heart Study, which supports a completely different conclusion about the effects of polyunsaturated oils on heart disease.
Not only does the evidence not support the claim that polyunsaturated fats prevent heart disease, it shows that just the opposite is true! The conclusion from the abstract:
Advice to substitute polyunsaturated fats for saturated fats is a key component of worldwide dietary guidelines for coronary heart disease risk reduction.
However, clinical benefits of the most abundant polyunsaturated fatty acid, omega 6 linoleic acid, have not been established. In this cohort, substituting dietary linoleic acid in place of saturated fats increased the rates of death from all causes, coronary heart disease, and cardiovascular disease.
An updated meta-analysis of linoleic acid intervention trials showed no evidence of cardiovascular benefit.
These findings could have important implications for worldwide dietary advice to substitute omega 6 linoleic acid, or polyunsaturated fats in general, for saturated fats. (Italics added.)
RELATED:
Profitable Cholesterol Drugs
It is a well-known fact that historically, drugs designed to lower cholesterol (statins) have been the most prescribed and most profitable drugs in the history of mankind. It is a $100 billion a year industry.
The cholesterol-lowering drug Lipitor is the best-selling drug of all time, grossing over $140 billion, with no serious close competitors in the history of pharmaceutical drugs.
It wasn’t until after the patent on Lipitor ran out, opening the door for cheaper generics to flood the market, that the FDA finally published warnings on the side effects of statin drugs, which include liver injury, memory loss, muscle damage, and Type 2 diabetes.
One out of every four Americans over the age of 50 is taking a statin drug to lower their cholesterol, so this is a huge market that depends upon the success of the lipid theory of heart disease which condemns saturated fats and cholesterol as bad.
How Many Lives Have Been Destroyed by Bad Nutrition Advice?
The science clearly shows how the “lipid theory of heart disease,” the belief that saturated fats and cholesterol cause heart disease, is false, but that science can never be published or exposed by Big Pharma, Big Food, or the U.S. Government.
To do so would be to admit that such dietary advice, and the cholesterol lowering drugs that have earned them hundreds of BILLIONS of dollars, have been a scam and have led to increased rates of obesity, diabetes, heart disease, and cancer.
These are the leading causes of death today.
The polyunsaturated edible oils consumed by over 90% of Americans today, which are not the edible oils of our ancestors, have replaced the traditional saturated fats that our ancestors consumed, such as butter, beef tallow, lard, and vegetable sources such as the tropical oils, coconut oil and palm oil.
Until recently, these recent additions to the human food chain, polyunsaturated oils derived from corn and soybeans, had to go through an industrial processing called “hydrogenation” to make them shelf stable and behave like saturated fats.
This process of hydrogenation was found out to be, years later, toxic, as it produced trans fats, which have now been banned in most countries, and require a warning on U.S. food labels.
In addition to the domination of these toxic vegetable oils, official USDA dietary advice, enforced by the FDA, encouraged a low-fat diet, resulting in the consumption of more carbohydrates, mostly in the form of refined sugar.
The fraudulent studies used to exonerate processed sugar and put the blame for heart disease and other diseases on saturated fat, has now been exposed.
The blood of millions of Americans who followed the advice from this faulty science used by the U.S. government now stains the hands of all those who corrupted the science, and the politicians who enforced it.
Written by Brian Shilhavy
Editor, Health Impact News
*Article originally appeared at Health Impact News; reprinted with permission