- SSRIs, which increase serotonin levels, have been linked to chronic fatigue syndrome (CFS). A study showed that administering Prozac (fluoxetine) to mice at high dosages induced symptoms of CFS, suggesting a link between excessive serotonin levels and the condition
- Symptom reversal was achieved with the serotonin inhibitor fenclonine
- Other serotonin inhibitors include Benadryl, the H2 blocker Pepcid (famotidine), aspirin, progesterone and GABA
- Branched-chain amino acids, tyrosine, phenylalanine, and L-theanine can also help reduce serotonin levels
- GABA is a more effective solution for conditions typically treated with SSRIs, such as depression and anxiety, without the adverse effects associated with elevated serotonin
- Reducing intake of linoleic acid (LA), found in high amounts in seed oils and certain meats, is recommended if you have CFS, as excess LA impairs your mitochondrial function and cellular energy production
Serotonin — also known as 5-hydroxytryptamine or 5-HT — is typically referred to as “the happiness hormone” and deficiency is thought to be the source of depression. That’s why depression is routinely treated with selective serotonin reuptake inhibitors (SSRIs) that raise serotonin levels in your brain.
The problem is, serotonin is NOT responsible for depression, and raising your serotonin is the last thing you want to do, as it destroys empathy, love and wisdom. Elevated serotonin also impairs thyroid function, reduces your metabolism, and contributes to premature aging by increasing reductive stress.
SSRIs Linked to Chronic Fatigue Syndrome
SSRIs have also been linked to chronic fatigue syndrome (CFS), otherwise known as myalgic encephalomyelitis (ME) or ME/CFS. As reported by bioenergetic medicine researcher Georgi Dinkov,1 elevated extracellular 5-HT has been shown to cause most of the CFS symptoms, including debilitating physical and mental fatigue.
“I am actually surprised it took researchers so long to make that connection,” he writes,2 “considering the well-tested so-called ‘central fatigue hypothesis’ (CFH), which stipulates that most of the perception of fatigue is brain-derived and often is not peripherally biochemically justified.
More specifically, it is the accumulation of serotonin in the brain, which leads one to perceive severe fatigue even if the bioenergetic state of their muscles do not demonstrate signs of fatigue (e.g. lactate buildup, creatine kinase and LDH leakage, ammonia accumulation, etc).
Conversely, lowering serotonin levels in the brain usually leads to abolishing the feelings of fatigue. In fact, there are multiple animal studies demonstrating that tryptophan depletion in the brain (which leads to lower 5-HT levels in the brain) is a reliable mechanism to delay or even abolish feelings of fatigue even in animals whose muscles are biochemically fatigued …
Another fact implicating 5-HT as a causal agent in CFS is the fact that most CFS patients seem to develop the condition as a result of viral infection … [M]ost viral infections require activation of specific 5-HT receptors (by elevated serotonin) in order for the infection to take hold, and blocking these receptors either prevents the infection altogether or can treat an already established one.”
One Month of Prozac-Induced CFS Symptoms in Mice
In one 2024 study,3 researchers were able to induce the classical signs and symptoms of CFS in mice by giving them Prozac (fluoxetine) for four weeks, albeit at dosages that are two to five times higher than what is used in clinical practice for depressive patients. Science Alert reported:4
“Based on clinical clues, Jin-Seok Lee, a ME/CFS researcher at Daejeon University in South Korea, and colleagues hypothesized that a spillover of serotonin could lead to ME/CFS. Known to play a role in governing moods, declining levels of the neurotransmitter serotonin have long been thought to cause depression.
Although that theory is now disputed, treatments that target serotonin pathways — such as selective serotonin reuptake inhibitors (SSRI) — are some of the most commonly prescribed antidepressants. By blocking receptors that bind and remove serotonin from the signaling pathway, the medication artificially maintains a higher level of the mood messenger.
According to several decades-old studies, some patients with ME/CFS appear to have fewer serotonin transporters than healthy volunteers and may also have receptors that only weakly bind serotonin.
Lee and colleagues thought that if such people had coincidentally been treated with serotonin-based treatments for depression before they developed ME/CFS, they may have had excessive levels of serotonin in their brain. This could have triggered ME/CFS by throwing off a feedback mechanism designed to keep a lid on the immune system and inflammation …
After four weeks, animals treated with fluoxetine had higher levels of serotonin in two parts of the brain, the hypothalamus and dorsal raphe nucleus.
They also developed behaviors that resembled the main symptoms of ME/CFS seen in humans, including unrefreshing sleep, PEM and orthostatic intolerance, but not cognitive impairment. These behaviors disappeared six weeks after the drug was stopped.
Mice whose serotonin receptors were depleted via viral knockout also showed ME/CFS symptoms, further confirming the mechanism. Another experiment showed inhibiting serotonin production could alleviate their symptoms.”
According to the authors:5
“Our study provides the first translational [animal] evidence for the involvement of 5-HTergic [serotonergic] hyperactivity in the pathophysiology of ME/CFS. With our novel animal model for ME/CFS, this study helps to clarify one of the potent pathophysiological mechanisms of this syndrome.
In addition, we provide diagnostic clues (high central serotonin) that can be used to differentiate ME/CFS from similar diseases, such as fibromyalgia and depressive disorders.”
Serotonin Inhibitors
The serotonin inhibitor used in the featured study was fenclonine, but there are several over-the-counter options as well, including Benadryl and the H2 blocker Pepcid (famotidine).
Aspirin can also lower extracellular serotonin by inhibiting the absorption of tryptophan from your gastrointestinal tract,6 while progesterone inhibits serotonin synthesis directly. Progesterone is one of only four hormones I believe many adults can benefit from. (The other three are thyroid hormone T3, DHEA and pregnenolone.)
As a general recommendation, I recommend most adults to take 25 to 50 mg of bioidentical progesterone per day, taken in the evening one hour before bed, as it can also promote sleep. For optimal bioavailability, progesterone needs to be mixed into natural vitamin E. The difference in bioavailability between taking progesterone orally without vitamin E and taking it with vitamin E is 45 minutes versus 48 hours.
Another good reason for taking progesterone with vitamin E is because it binds to red blood cells, allowing the progesterone to be carried throughout your body and distributed to where it’s most needed.
Simply Progesterone by Health Natura is premixed with vitamin E and MCT oil. You can also make your own by dissolving pure USP progesterone powder into one capsule of a high-quality vitamin E, and then rub the mixture on your gums. Fifty milligrams of powdered progesterone is about 1/32 teaspoon.
Do not use synthetic vitamin E (alpha-tocopherol acetate — the acetate indicates that it’s synthetic). Natural vitamin E will be labeled “d alpha-tocopherol.” This is the pure D isomer, which is what your body can use. There are also other vitamin E isomers, and you want the complete spectrum of tocopherols and tocotrienols, specifically the beta, gamma, and delta types, in the effective D isomer.
I do not recommend transdermal progesterone, as your skin expresses high levels of 5-alpha reductase enzyme, which causes a significant portion of the progesterone you’re taking to be irreversibly converted primarily into allopregnanolone and cannot be converted back into progesterone.
GABA Is a Far Better Choice Than SSRIs
It’s a travesty that the primary remedy for depression is a drug that not only comes with a laundry list of side effects such as CFS, but also doesn’t address the underlying problem in the first place. Again, depression is not the result of low serotonin.
GABA is a more effective solution for conditions typically treated with SSRIs, such as depression and anxiety, without the adverse effects associated with elevated serotonin.
A far more common problem in depression is GABA deficiency, and increasing GABA can indeed be part of the solution. As explained by Dr. Scott Sherr, director of integrative hyperbaric medicine and health optimization at Hyperbaric Medical Solutions and an expert on neurotransmitter balancers like GABA:
“GABA deficiencies are associated with anxiety, with fear, with depression, with a short temper, phobias, impulsiveness, disorganization, addictions. It’s even associated with schizophrenia and OCD [obsessive-compulsive disorder].
You can also have things like IBS and diarrhea, hypertension, tinnitus, chronic pain, migraines, allergies, frequent urination, flushing, sweating, salt cravings, muscle tension. These are all things that could be signs of GABA deficiency. Many have been prescribed an SSRI for some of these symptoms, but … we know that depression is not related to serotonin deficiency.”
In my view, GABA is one of the easiest solutions for depression, anxiety and insomnia, either alone or with progesterone. I recommend a dose of 500 mg to 2,000 mg (2 grams) daily. This range has been shown to relieve anxiety and insomnia in people who are already taking SSRI drugs.
However, according to Sherr, as little as 100 milligrams of GABA has been shown to lower the assessment scores of patients with anxiety and depression disorders. Effects can be further amplified by combining it with the amino acid L-theanine, which is a natural GABA agonist.
Just be careful using GABA products that contain magnesium. While magnesium is very helpful, if you take high doses of GABA, you will get far too much magnesium, which can have a laxative effect.
Interestingly, if you take too much GABA, some of it will get deaminated and convert into succinic acid, an intermediate of the Krebs cycle. As such, GABA also helps boost mitochondrial function at high doses. So, from a toxicity perspective, it appears to be very safe.
To Address CFS, Be Sure to Eliminate LA
As for CFS sufferers, the No. 1 remedy would be to drastically lower your daily LA intake, as excess LA acts as a mitochondrial toxin and severely inhibits cellular energy production. Naturally, if your cellular energy production is low, you’re going to struggle with fatigue and a host of other health problems. PUFAs like LA also disrupt your body’s hormonal equilibrium, imitating the effects of estrogen and cortisol while counteracting androgens and progesterone.
Considering the profoundly serious damage they cause, eliminating seed oils from your diet can go a long way toward improving your health. This includes soy, canola, sunflower, grapeseed, corn, safflower, peanut and rice bran oil.
Also, be mindful of olive oil and avocado oil, as both are commonly adulterated with cheaper seed oils. That said, even pure olive and avocado oil are loaded with LA. If, like me, you’re in the habit of eating olive oil, I would strongly encourage you to limit your intake to 1 tablespoon per day or less. In my view, olive oil is not a magic bullet and if you are already consuming 80 grams of LA per day, it will only worsen, not help, your health.
To avoid these oils, don’t cook with them, of course, but also avoid processed foods, condiments, fast foods and restaurant foods. If you eat out, you’re undoubtedly eating unhealthy amounts of seed oils, as most restaurant foods are loaded with it.
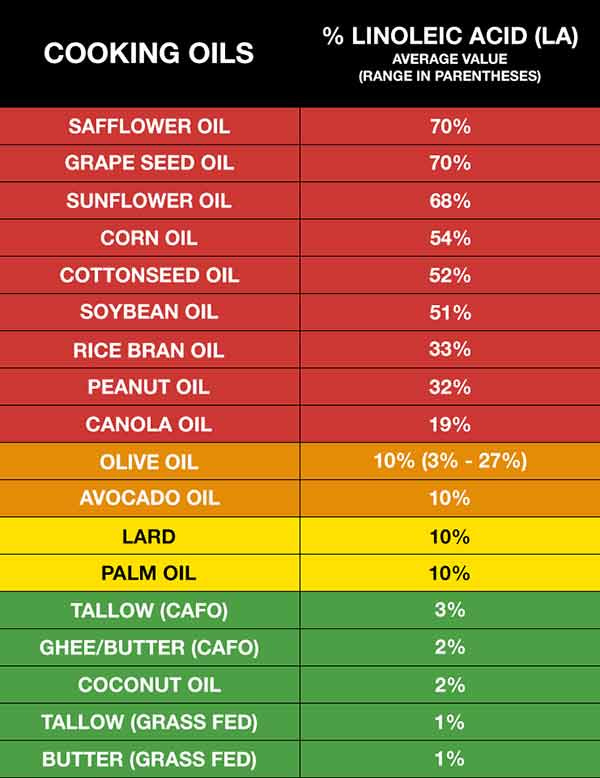
Fried foods, dressing and sauces tend to be key culprits. Your best bet is to prepare most of your food at home, so you know what you are eating and, in the case of seed oils, what you’re not. Chicken and pork are also high in LA and are therefore best avoided. Since these animals, even healthy organically grown animals, are typically fed grains, they are loaded with omega-6 fats and may have 10 times the LA content that beef, lamb or buffalo do.
How Much Linoleic Acid Is Too Much?
Ideally, consider cutting LA down to below 5 grams per day, which is close to what our ancestors used to get. If you’re not sure how much you’re eating, enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake.
The key to accurate entry is to carefully weigh your food with a digital kitchen scale so you can enter the weight of your food to the nearest gram. Cronometer will tell you how much omega-6 you’re getting from your food down to the 10th of a gram, and you can assume 90% of that is LA. Anything over 5 grams is likely to cause problems.
ORIGINALLY PUBLISHED BY: DR. JOSEPH MERCOLA.
Sources and References